Taking the Complexity Out of the Shoulder Complex
By: Jiaqi Yan, B.Sc Kin, MScPT student; Edited by Nataliya Zlotnikov, MSc, HBSc ∙ Estimated reading time: 8 minutes
By: Jiaqi Yan, B.Sc Kin, MScPT student; Edited by Nataliya Zlotnikov, MSc, HBSc ∙ Estimated reading time: 8 minutes
Do You Know Why Shoulder Injuries are So Common?
The shoulder is one of the most commonly injured structures in our body.The unique and complex anatomy of the shoulder makes it the joint with the greatest range of motion—great for carrying the weight of the world—but the least stability. Thus, it is more susceptible to strain, repetitive injuries, and aging than other joints (Rush University, 2022).

Taking the Complexity Out of the Shoulder Complex
Because the shoulder relies heavily on surrounding muscles, ligaments, and joints, shoulder pain often originates elsewhere in the body. Dysfunction in the neck, spine, or even breathing patterns can all contribute, making assessment challenging.
A standardized, hierarchical approach helps remove guesswork. By first looking at the big picture and then narrowing the focus, clinicians can more accurately identify the true source of a shoulder issue and improve outcomes.
The Neck is Number One
When it comes to the shoulder, the neck takes priority, meaning we must clear the cervical spine and neurological structures before anything else. This is of utmost importance as we can differentiate whether a client’s shoulder complaints are coming from upstream (e.g. limited c-spine rotation compromising the shoulder), or if it is a neurological issue rather than a musculoskeletal one.
Once we clear the neurological structures, we can then move through the hierarchy of the 7 Principle Pillars of a healthy shoulder.
This blog provides an overview of the 7 Principle Pillars of a healthy shoulder. The 7 Pillars are discussed in greater detail in these two great courses from PT, Tom Swales’ on Embodia, the introductory A Hierarchical Approach to Assess, Treat, & Prescribe for the Shoulder, and The Ultimate Guide to Shoulder Health Workshop.
The Ultimate Guide to Shoulder Health Workshop delves into:
- Quick screening for mobility imbalances
- The 7 Principle Pillars for a healthy shoulder and 3 Practical Pillars
- Corrective exercise techniques with the use of foam rollers, bands, kettlebells, and body weight exercises
- Progressive mobility and strength program for the shoulder girdle complex, hips, and thoracic spine
- Progressive exercise techniques to safely perform the strict muscle-up on the Olympic rings and straight bar
- Participants will receive a small booklet of the exercises taught with brief descriptions of each so they can continue to practice safe effective techniques.
A Hierarchical Approach to Assess,
Treat, & Prescribe for the Shoulder
The Ultimate Guide to Shoulder Health Workshop
7 Principle Pillars of a Healthy Shoulder

1. Breath
Breath is the foundation, without it, there is no life.
We begin and end our life with the breath, taking between 17,000 and 30,000 breaths per day.
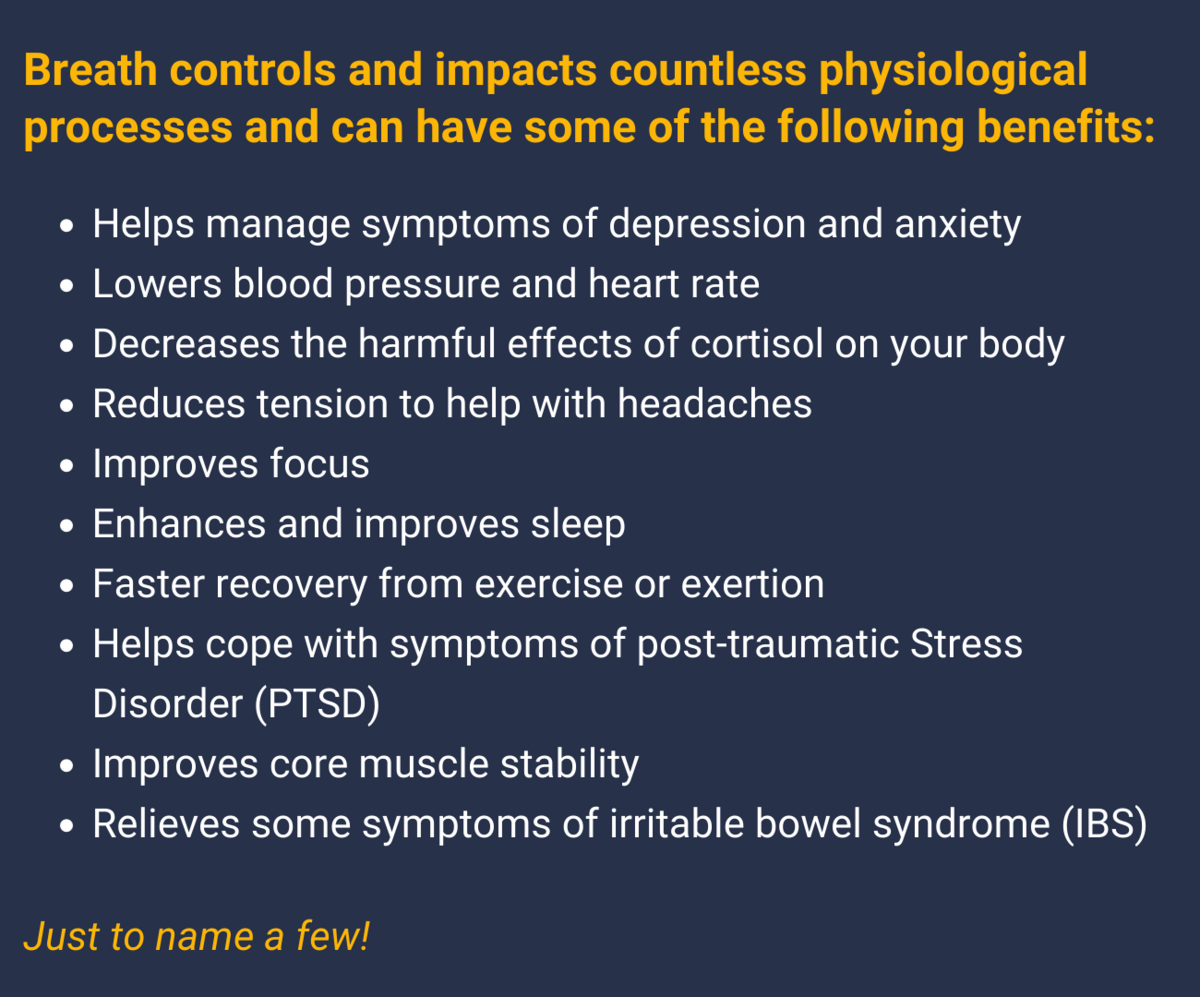
As rehab professionals we know how important the breath is, but do we always remember to check how our clients are breathing?
Suboptimal breathing patterns can result in problems for the shoulders. Checking our client's breathing by looking for any suboptimal breathing patterns is a crucial step in treating the shoulder!
A few of these breathing patterns include, but are not limited to:
- Fast/shallow breathing
- Use of accessory muscles
- Mouth breathing
- Paradoxical breathing
For example, if a client is shrugging with each breath, it can create large amounts of tension in the neck, trapezius, and shoulders.
By incorporating proper breathing, we can calm down the nervous system, decrease inflammation and move away from a sympathetic state. Together, this allows for less pain and more energy to prepare patients to complete their rehabilitation exercises.
Breathing also acts as an opportunity to teach patients to be more mindful and aware of their body, movement patterns, and habits.
2. Posture/positioning
![]()
Our posture is a physical representation of the input from our external and internal environments.![]()
Our internal mindset can affect our posture! You’ve seen happy, confident clients walk into your office with a sort of ‘power stance’, standing tall, chest open; if someone is low energy, they tend to be slouched, have shallow breath, and speak quietly.
An example of an external environment affecting posture is temperature, if people are too cold, they also tend to hunch over.
A lot of posture has to do with a lack of stimulation! How many of our clients (or us) get stuck working on our computers for the whole day, staring at a screen, and reverting to this sort of hunched-fetal position?

A lack of external stimulation can negatively affect our posture and paralyze our movement literacy by being stuck in a certain body position for an extended period.
How do we get our clients out of that hunched-over fetal position and get extended and tall? We help them stimulate the cerebellum!
Stimulating the cerebellum can include things such as going on the stomach, doing eye exercises, looking around, etc. These movements will create that spinal extension that we are looking for.
You can have your clients sit on the floor. This will open up their hips and gets people to fix their postures. But if you simply have your clients try to sit there and muscle their posture away - they will lose.
Getting a client into their ideal posture is essential, resulting in improved ease and quality of movement. Thus, movement strategies when it comes to rehabbing the shoulder will become easier to structure.
3. Grip
![]()
We are connected to the environment and objects through our hands. ![]()
The hand and shoulder work through the grip reflex, specifically, the irradiation reflex. That is, the more tension created in a muscle, the greater the tension in the surrounding muscles and kinetic chain will be.
With a strong grip, the shoulder becomes more “packed in” and stable. Engaging a strong grip protects the joints, as the shoulder won’t take seriously what the grip doesn’t.
With a loose grip, the shoulder will be “loose” in that it becomes less stable and easier to dislocate.
It is best to measure grip using a hand grip dynamometer as we aim to have less than a 5 kg difference between limbs. The asymmetry in grip strength can result in overuse injuries in the shoulder when doing bilateral upper body movements as the stronger side will automatically compensate.
Additionally, we can measure grip strength in various shoulder positions to identify the areas in which the shoulder is weak and has decreased neural output. Locating shoulder positions where the grip is weak can tell us that extra work needs to be done in these areas and that these positions should be targeted when it comes to treatment planning.
4. Thoracic spine mobility
![]()
The ribcage is a mobility joint, and we need to make sure that it bends, twists, side bends and rotates. ![]()
But because our patients (and we) get fixed into these hunched positions and lose extension, they’re not rotating as they should. Now all of a sudden, because they can’t rotate, this will impact the scapula and we might find our patients rotating a bit more through the shoulder, placing more stress on the tissues.
So we must make sure that there is sufficient mobility in the t-spine as this will allow for an optimal position for scapular stabilizers, ensure proper scapular movement, expand and rotate the ribs and stabilize the spine.
But let’s not forget our breath (Pillar #1). Breathing and thoracic mobility highly influence each other, if your patient is still displaying any suboptimal breathing patterns such as mouth breathing, those ribs are going to chronically be stiff.
If breathing is not fixed, we must go back to it.
How can we help our clients improve their t-spine mobility?
We can include the following in our client’s rehabilitation programs:
- Thoracic extension and breathing
- Fascial flossing: Latissimus/Teres major
- Active mobility progressions
5. Scapular control
![]()
We need to improve scapular control and proprioception through all the planes that are available to us.![]()
The entire rotator cuff sits on the scapula, if the scapula is not in the right position, exercises that involve the use of the shoulder, such as a push-up, for example, will only result in the scapula tipping and further compromise the shoulder, increasing the risk of injury.
Therefore scapular control, proprioception, and straight arm strength in all planes must be set first to allow for efficient shoulder movement.
As a reminder, the scapular movements consist of:
- Protraction
- Retraction
- Elevation
- Depression
- Upward/downward rotation.
Make sure the scapula can effectively perform all of these movements and target the areas that are lacking.
Here are a few exercises that you can use in your practice to help your patients develop and improve scapular proprioception and control:
- Proprioception: Quadruped scapular circles, ABCs
- Scapular retraction: Wall slides, scap rows
- Protraction: Serratus slides, banded or ball ABCs
- Quadruped scap-lock rotations: HBH rotation, SB sit backs to lock lumbar spine
6. Spine stability
![]()
The shoulder sits on top of the thorax and pelvis. If the pelvis is out of whack, it doesn’t matter what you do to the shoulder, its not going to get better because you haven’t fixed the alignment of the spine yet.![]()
We have to set these things in place to have greater outcomes for our patients’ shoulder rehabilitation.
Our core plays a key role in increasing the stiffness of the spine and transferring load through the limbs, from hip to shoulder and shoulder to hip.
In other words, a strong core acts as a stable base for the shoulder to work on especially when performing our daily activities, as it essentially is involved in every movement we perform whether it be unconsciously or consciously.
As an example, a client who is constantly in a side bend position lacks spine stability and oblique core strength, which can negatively impact the shoulder.
There are 3 primary core exercises: the dead bug, bird dog, and side plank, each with its set of progressions that will collectively target all of the global muscles of the core and increase the stiffness of the spine.
When performing these exercises, it is essential to activate the deep core system before performing the movement. We want to “set up” the core to increase our spinal stability beforehand and this can be accomplished by incorporating the breath.
The cueing that can be taught when it comes to setting up the deep core is “breath, set, move”. Take a deep breath through the nose and out through the mouth, at the end of the exhale set the deep core muscles, and then proceed to perform the movements.
7. Glenohumeral Joint
Lastly, once all those 6 are in place, now, let’s look at the shoulder!
When we take care of the other 6 pillars, we are setting up the shoulder to perform optimally and decrease the risk of injury.
A lot of the time once we’ve gone through these first 6 pillars and then we retest the rotator cuff, we’ll notice that it is suddenly much stronger, but we haven’t done anything to it! We’ve just provided the input to change the output (the strength of the rotator cuff).
The focus for the shoulder should be on strength and mobility.
Here are a few things you can do to target shoulder strength and mobility:
- For strength, we can easily isolate shoulder structures by performing dumbbell raises in multiple directions, or directly target the rotator cuff by performing external/internal rotation with resistance bands.
- For mobility, shoulder proprioception circles are a good way to get clients moving in a range they may have avoided. Getting them to achieve greater ranges is beneficial for long-term pain and mobility.
- Additionally, dowel lifts are an excellent way to address fascial and joint restrictions in the shoulder. Particularly, shoulder extension with a dowel, as most of our daily activities require our shoulders to be in a flexed position. Increasing shoulder extension range can promote safer loading in this position, where a lot of our shoulder injuries occur.
A Hierarchical Approach to Assess,
Treat, & Prescribe for the Shoulder
The Ultimate Guide to Shoulder Health Workshop
Conclusion
We hope the hierarchical approach introduced in this blog takes the complexity out of the shoulder complex and that you can apply the pillars discussed in your practice.
As this blog is all about structure, we feel it is only fitting to end on that note as well and leave you with some final do’s and don'ts:

---
Date written: 7 July 2022
Last update: 15 December 2025

MPT, ACT, FCAMPT, AMTC, CSCS
Tom Swales is a practicing physiotherapist and strength coach with a particular focus on human movement. He is the founder and creator of Swales Performance Systems (SPS), which educates advanced knowledge of human movement. Toms work and ideas are at the forefront of fitness, conditioning, injury prevention and rehabilitation.
Tom completed his Bachelor of the Arts in Athletic Training with honours at Graceland University in Lamoni, Iowa while on a soccer scholarship in 2002. He continued on to complete his Masters of Physiotherapy at the University of Western Ontario in 2006. He holds many advance diplomas and certifications specializing in manual therapy, acupuncture, strength and conditioning and concussion management. He has been a physiotherapist and strength coach for the Canadian Men’s Alpine Ski Team, a Lead Medical Practitioner for Soccer at the TO Pan Am Games as well has a loyal clientele of elite / professional athletes.
Tom’s treatment philosophy includes using manual techniques, acupuncture to restore normal joint and soft tissue mobility, then supplementing it with functional corrective exercise techniques and movement strategies to prevent injury re-occurrence. Patient education on their injury and understanding of how and where movement is produced is an integral part in our treatment philosophy and preventive strategies.
Through his work, Tom has the vision to empower people and help them gain confidence in their potential and abilities. His whole body approach and empathetic character complement his extensive experience perfectly, allowing him to guide his clients through their issues and through the challenge of achieving the healthy bodies they deserve.
Tom teaches his approach to fellow professionals in the health and wellness industry to offer workshops in movement foundations and whole body exercise therapy. Toms integrated knowledge across the fields of human movement, strength and performance has given him the foundation to create a user-friendly framework for assessment and prescription of exercise for all types of physical mobility impairments.
Tom’s social life is busy, filled with clinical work, speaking engagements, writing, self-enhancement and family time with his wife and two young children.
Checkout Tom’s professional development site: https://www.tomswales.com
